Blog article
The Kegel Chronicles – A postpartum guide to building pelvic floor strength with a Women’s Health Physio

Meet HBF Physio’s Danica. With a Masters in pelvic health, she’s here to provide some expert insight into
the benefits of working with a women’s health physio in your postpartum months and a bit about what you can
expect from your initial appointments — including a workout you’ll want to get in the Mother’s
Group WhatsApp chat pronto.
We’ll walk you through a month of pelvic floor-focused exercise and nutrition, and how a
tailored plan can help you feel confident returning to exercise and keeping up with all that life as a new mother
entails. Consider it a small reminder to make a physio appointment but a big reminder that you are doing
great.
Depending on your pregnancy and delivery, you may be experiencing:
- Pelvic Pressure or Heaviness: A feeling of "something falling out" or a bulging in the vagina.
- Pelvic Pain or Aching: Generalized discomfort in the lower pelvis that may feel worse with standing or sitting for a long time.
- Urinary Symptoms: Leaking urine, urgency, or difficulty starting urination – this is often due to weakened or overworked pelvic floor muscles from pregnancy or childbirth.
- Bowel Symptoms: Don’t forget the bowels – they are included in all this! Constipation, pain during bowel movements or fecal incontinence may be experienced postpartum.
- Muscle Tightness or Spasms: The pelvic floor can become overly tight (hypertonic) from trying to protect or compensate after injury.
This is all in the realms of what a women’s health physio can support you with.
Step One: Getting to know your Physio, and your pelvic floor
Your initial appointment is an important one. If you didn’t work with a Physio during pregnancy, you may be a
stranger to a pelvic floor exam via ultrasound. In postpartum, to help create a plan tailored to your needs, an
internal vaginal examination may also be performed.
Danica says this is the best way to accurately assess the pelvic floor for; baseline strength, endurance (how long you
can hold a contraction) functionality (how well you can contract and relax the pelvic floor), vaginal prolapse, and
any tender or tight areas.
Once you have made an informed decision and consented to the exam your physio will assess the resting tension of the muscles, ask you to contract and relax the muscle several times as well as assess what your pelvic floor does under strain (eg. cough, sneeze, bearing down). The results of this assessment will be used to create a targeted program, with everyone’s being a little different.
Step Two: It’s about squeezing (so you don’t fear sneezing)
But first, a diagram. This is your pelvic floor.
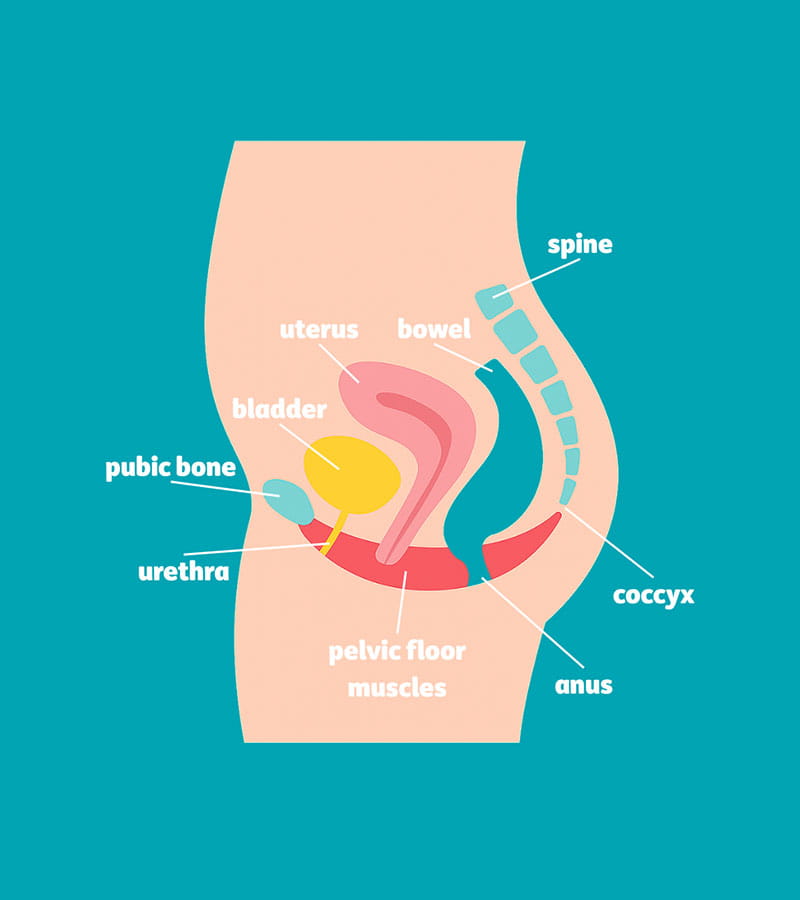
Now that you know what it looks like, let’s talk about how your physio will design exercises tailored to your history. You’re looking at a powerful mix of basic Pilates, moving up to high-impact exercises, topped off with empowerment.
Here’s how Danica from HBF Physio works with her postpartum clients:
- Tailored Pelvic Floor Exercises: Specific exercises to strengthen weak muscles– pelvic floor exercises (Kegels) aimed at overloading your muscles to improve strength and function or, in the case of overactive pelvic floor muscles, techniques to relax and lengthen them.
- Manual Therapy: Hands-on techniques to release muscle tension, scar tissue, or adhesions (especially helpful after tearing, episiotomy, or C-section). Gentle internal work may be used to improve mobility and reduce pain.
- Bladder and Bowel Retraining: Techniques to improve bladder control, reduce urgency, or manage constipation. Education on proper toileting posture and habits.
- Core and Posture Rehab: Training in safe abdominal and core activation, especially if you have diastasis recti (separated abdominal muscles). Guidance on posture, breathing, and body mechanics to reduce pressure on the pelvic floor.
- Pain Management: Help with perineal pain, vaginal dryness, or pain during intercourse. Use of techniques like desensitization, biofeedback, breathing, and relaxation exercises.
- Education and Empowerment: Learn about what’s normal, what to expect during recovery, and how to safely return to exercise, sex, and daily activities. Danica also likes to provide support for emotional well-being, acknowledging how pelvic discomfort can affect mental health.
When it comes to returning to exercise, it’s all about going back to the basics to begin with; pelvic floor control, abdominal/core control and hip/lower limb control. Whether it is through a supervised home-based program or group exercise setting such as pilates, working on the foundations and then gradually progressing is important.
“There is so much pressure on new mums to “bounce back”. We need to remember that pregnancy changes occur over a 10-month period and labour has a significant impact on our bodies. Return to exercise should be looked at as a marathon not a sprint. A lot of women are not ready to return to high impact activity or sport at 6 weeks and that is ok.” Says Danica
If you're thinking about growing your family again, it's the perfect time to check in with your body — especially your pelvic floor. Even if your first postpartum year didn’t include structured rehab (hello, survival mode) you can still build a stronger foundation for pregnancy #2 (or #3, or #4). Once again, it’s all about going back to basics; reconnect with your core and pelvic floor, address any lingering symptoms (heaviness, leaking, weakness) and learn strategies to support your body during pregnancy and birth.
Reminder: It’s never too late to start. Recovery and readiness aren’t about where you’ve been – both are about where you’re going.
Step Three: Nutrition – yes, you can still drink coffee
It’s important for an element of nutrition to come into your pelvic floor plan – and knowing your triggers is what makes all the difference.
Ensuring you consume enough fibre and fluids is important and reducing known bladder irritants (caffeine, alcohol, carbonated beverages, acidic food) can make the world of difference to pelvic floor symptoms.
“Your pelvic floor deserves a nutrition plan as personal as your taste in coffee – know your triggers, fuel your body, and yes, you can still sip that latte!”
Step Four: Keep on going. (What a difference a month can make!)
Ok, ready for your postpartum pep talk? Here goes.
Yes, you can make noticeable changes to your pelvic floor strength in one month—especially if you’re consistent and intentional with your exercises. While full muscle retraining can take a few months, many people begin to notice improvements within 3 to 4 weeks.
What You Can Achieve in One Month:
- Improved muscle awareness – Learning to correctly activate and relax your pelvic floor.
- Better bladder control – Especially with stress incontinence (leaking when coughing or sneezing).
- Increased endurance – Holding contractions longer.
- Reduced symptoms – Like heaviness, urgency, or mild prolapse discomfort (in some cases).
So – book in with a physio, start those exercises, write down your progress – and call it the Kegel Chronicles!
To get you started, here’s a simple Kegel from Danica you can do in the car, the bath or even in bed.- Get comfy – Sit or lie down with your body relaxed
- Take a deep breath into your belly, breathe all the way out
- Imagine you’re stopping wee mid-flow or trying to hold in wind – Gently squeeze the muscles you’d use to do that. Don’t clench your bum, thighs or tummy — it’s all internal
- Hold the squeeze for 3 seconds while breathing normally
- Release slowly and fully relax for 5–10 seconds
- Repeat 10 times.
Pro tip: Pair it with red lights (in the car), a few deep breaths (in the bath), or the end of a Netflix episode (in bed). Small moments = real results.
Some FAQs to save you from a 3am googling session
Q: Should I hold on when I need to wee, does that help my pelvic floor?
Short answer: No, and please don’t!
Longer answer: Holding your wee regularly can actually confuse your bladder signals and may lead to issues like urgency or incomplete emptying. It doesn’t strengthen your pelvic floor – in fact, it might just add more stress. Instead, respond to your body’s natural cues, and focus on your individualised pelvic floor exercise program
Q: I still feel a heaviness one year postpartum, is this normal?
Short answer: It’s common, but not normal and it is not something you have to just “live with.”
Longer answer: A feeling of heaviness or pressure could be a sign of pelvic organ prolapse or ongoing pelvic floor muscle weakness. Even a year or more postpartum, your body has a remarkable capacity to heal and improve with the right support. A pelvic health physiotherapist can assess what’s going on and guide you to effective recovery – it’s never too late.
Q: I want to have a second baby but my pelvic floor is weak, can I get it back and ready for round two if I didn’t exercise during my first year postpartum?
Short answer: Absolutely – it’s never too late to start.
Longer answer: Even if you didn’t focus on pelvic floor muscle training during your pregnancy or postpartum, you can still build strength and support before your next pregnancy. With a bit of consistency, proper guidance, and maybe some professional help, your pelvic floor can bounce forward (not back) and be more prepared than ever for round two.
So, the next time you give your beautiful baby a gentle loving squeeze, think about who else might enjoy the same (your pelvic floor) and if you feel ready to make a plan on getting back to exercise and strengthening your pelvic floor – a women’s health physio can help.
This article contains general information only and does not take into account the health, personal situation or needs of any person. In conjunction with your GP or treating health care professional, please consider whether the information is suitable for you and your personal circumstances.




